Bilateral Oophorectomy Procedure: Comprehensive Guide
The bilateral oophorectomy procedure is a significant surgical intervention that involves the removal of both ovaries. This procedure is often recommended for various medical reasons, including the treatment of certain cancers, endometriosis, and other ovarian-related conditions. In this article, we will delve deeply into the details of the bilateral oophorectomy, including its indications, the surgical process, potential risks, recovery, and the overall impact it has on patients' health and well-being. Insights from experienced professionals like Dr. Seckin can help enhance understanding and decision-making regarding this critical health procedure.
What is a Bilateral Oophorectomy?
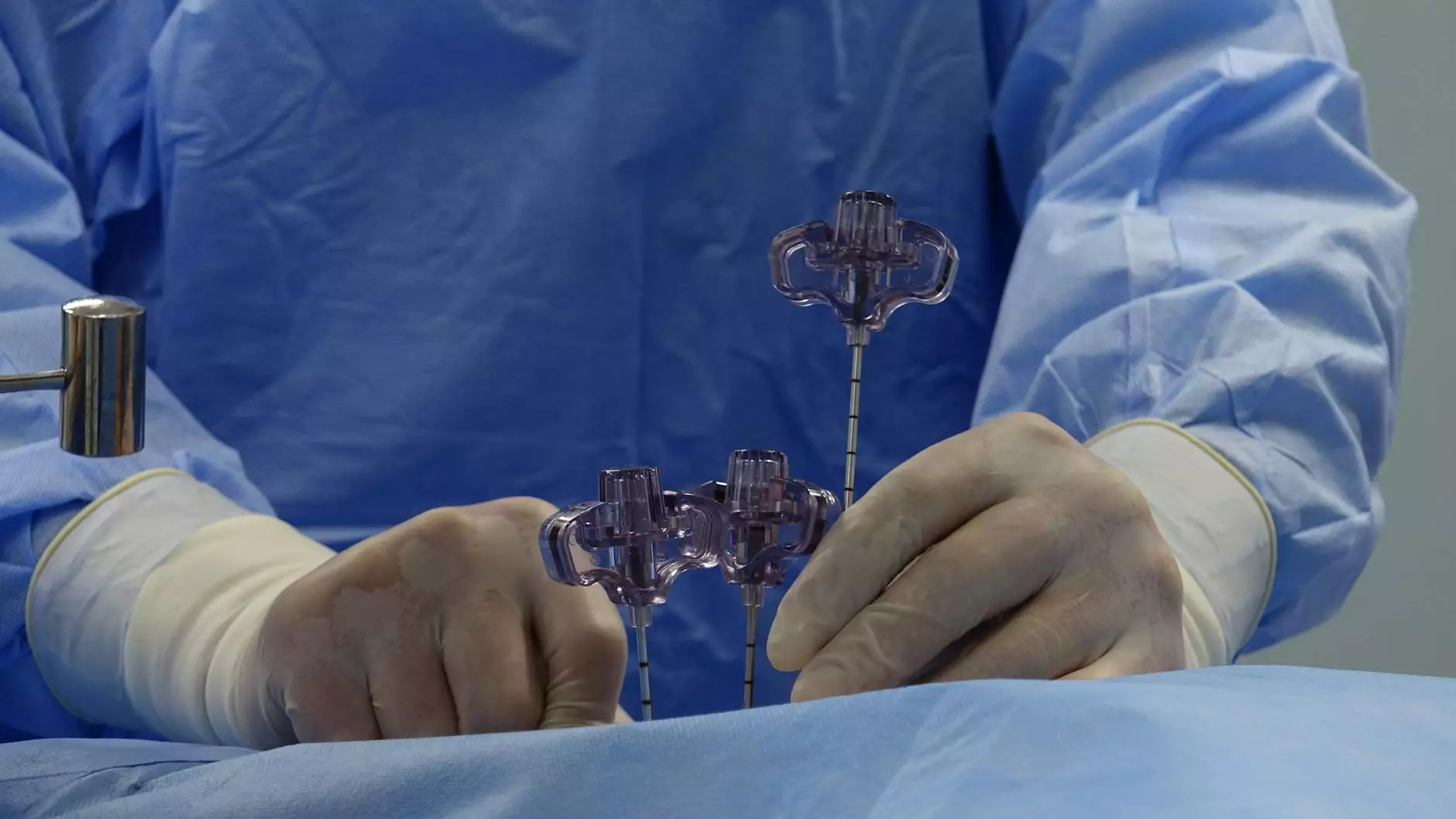
A bilateral oophorectomy involves the surgical removal of both ovaries. The ovaries are female reproductive organs responsible for producing eggs and hormones such as estrogen and progesterone. This procedure is typically performed using laparoscopic techniques or through an open surgical approach, depending on the patient's specific circumstances and the underlying reasons for the surgery.
Indications for Bilateral Oophorectomy
The decision to undergo a bilateral oophorectomy is primarily based on various medical indications. Some of the most common reasons for this procedure include:
- Ovarian Cancer: A primary indicator for a bilateral oophorectomy is the presence of malignant tumors in one or both ovaries. Early-stage ovarian cancer may only require the removal of the affected ovary, but advanced stages typically necessitate a bilateral approach.
- Endometriosis: Severe endometriosis can lead to significant pain and infertility. In cases where other treatments have failed, a bilateral oophorectomy may be recommended.
- Genetic Predisposition: Women with BRCA1 or BRCA2 gene mutations may opt for this procedure to markedly reduce the risk of developing ovarian and breast cancer.
- Ovarian Cysts: Recurrent or problematic cysts may necessitate removal for diagnosis and treatment purposes.
- Hormonal Imbalance: In some cases, the ovaries may cause hormonal imbalances leading to health issues; removal can alleviate these problems.
The Bilateral Oophorectomy Procedure: What to Expect
Pre-Operative Assessments
Leading up to the surgery, patients will undergo a series of pre-operative evaluations, including:
- Complete blood tests to assess overall health
- Imaging studies like ultrasounds or CT scans to understand the condition of the ovaries
- A thorough discussion of medical history and potential risk factors with the healthcare provider
The Surgical Process
On the day of the procedure, patients are typically referred to a surgical center or hospital for their bilateral oophorectomy. The steps generally include:
- Anesthesia: The procedure is performed under general anesthesia, ensuring that patients remain unconscious and pain-free throughout the operation.
- Incisions: For a laparoscopic procedure, small incisions are made in the abdominal wall. If an open surgery approach is necessary, a larger incision may be made.
- Removal of Ovaries: The ovaries are carefully detached from their attachments and removed. If needed, other reproductive organs may also be removed.
- Closing Incisions: Once the ovaries are removed, the incisions are closed, typically with sutures which may dissolve over time.
Post-Operative Care and Recovery
Post-surgery, patients will be monitored for a period before being discharged. The recovery process varies from person to person but generally includes:
- Rest: Patients are advised to take sufficient rest and avoid strenuous activities.
- Pain Management: Pain medication may be prescribed to manage discomfort.
- Follow-Up Appointments: Scheduled follow-ups are essential for assessing recovery and addressing any complications.
Potential Risks and Complications
Like any surgical procedure, a bilateral oophorectomy carries potential risks. These can include:
- Infection: There is a risk of infection post-surgery, which may require antibiotics or additional treatment.
- Bleeding: Patients may experience excessive bleeding, necessitating transfusions or further procedures.
- Damage to Surrounding Organs: The surgical manipulation may inadvertently affect nearby organs such as the bladder or intestines.
- Hormonal Changes: Removal of the ovaries leads to immediate surgical menopause, which can result in symptoms such as hot flashes, mood swings, and vaginal dryness.
Impact on Long-Term Health
The long-term implications of a bilateral oophorectomy can significantly affect a woman's life. The absence of ovaries leads to the cessation of hormone production, which can prompt various physical and emotional changes:
- Menopausal Symptoms: Women may experience a range of menopausal symptoms sooner than natural menopause.
- Bone Health: Decreased estrogen levels can affect bone density, leading to osteoporosis concerns.
- Heart Health: Hormonal changes might influence future heart health, emphasizing the importance of regular check-ups.
Managing Hormonal Changes
To address the hormonal changes post-surgery, many women may consider hormone replacement therapy (HRT). HRT can help alleviate menopausal symptoms and provide health benefits in bone density and heart health. However, it is essential to discuss the potential risks and benefits of HRT with a healthcare provider before making a decision.
Conclusion
The bilateral oophorectomy procedure is a complex yet crucial intervention for women facing serious health challenges related to their reproductive health. Understanding the reasons for surgery, what to expect during the operation, and the recovery process can empower women to make informed decisions. The expertise of providers like Dr. Seckin can guide patients through this journey, ensuring that necessary precautions and supportive care are provided.
Women considering a bilateral oophorectomy should engage in comprehensive discussions with their healthcare professionals to explore their options, understand the implications, and plan for a healthy future.